What is glaucoma?
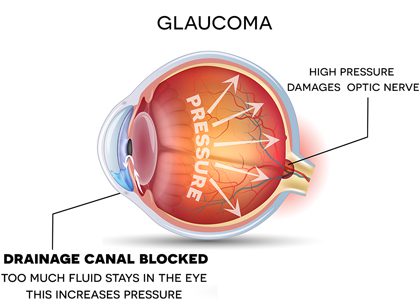
Glaucoma is a group of eye diseases that damage the optic nerve. Most forms of glaucoma are associated with high intraocular pressure (IOP), but the disease can also develop in people with normal or low eye pressure.
How does glaucoma affect vision?

The purpose of the optic nerve is to transmit visual signals to the brain. In glaucoma patients, pressure builds inside the eye and gradually causes damage to the optic nerve. This causes the link between the eye and the brain to break over time. If visual information can’t be sent to the brain via the optic nerve, the result is permanent blindness.
Known as the “silent thief of sight,” glaucoma advances slowly over many years. There are typically no warning signs or symptoms of vision loss in people with early stage glaucoma. If the disease is not detected and treated as soon as possible, glaucoma can cause irreversible vision loss.
What are the types of glaucoma?
Open-Angle Glaucoma is the most common form of glaucoma. The disease develops slowly with age and affects the drainage canals in the eye, which become clogged over time. Most people do not notice early symptoms because glaucoma attacks peripheral vision before it affects central vision.
Angle Closure Glaucoma happens suddenly and rapidly, with no warning. It is caused by a buildup of fluid in the eye — the inability for the fluid to drain causes a rapid increase in eye pressure, which has an immediate effect on the optic nerve. Common symptoms include severe eye pain or headaches, sudden loss of vision, blurry eyesight, and nausea. These symptoms may indicate a medical emergency and must be treated immediately to avoid severe vision loss.
Fortunately, prompt laser treatment and medications can clear the fluid blockage and lower eye pressure in people with angle closure glaucoma.
Low or Normal Tension Glaucoma is typically diagnosed when people with normal eye pressure experience optic nerve damage or peripheral vision loss. Unfortunately, there is not enough research to explain what causes damage to the optic nerve if eye pressure is within the normal range.
Congenital Glaucoma is a form of glaucoma in which children are born with a defect in the angle of the eye that interferes with fluid drainage and eye pressure levels.
Secondary Glaucoma occurs as a result of other diseases or medical treatments, such as:
- High blood pressure
- Poorly managed diabetes
- Cataract complications
- Uveitis
- Steroids
Can glaucoma be prevented?
Glaucoma cannot be prevented; however, early detection and treatment can help to control the disease before severe vision loss occurs. For adults over the age of 40, ophthalmologists recommend scheduling an annual comprehensive eye exam that includes pupil dilation. Since glaucoma typically affects peripheral vision first, you may not notice any changes to your prescription, which makes annual exams all the more important. Your eye doctor will test your vision, check your eye pressure and the condition of your optic nerve during the exam.
Am I at risk for glaucoma?
Glaucoma affects nearly three million Americans. Some groups of people are at a higher risk of developing the disease than others.
It is especially important for these groups to schedule annual eye exams to check for early stages of glaucoma:
- African Americans
- Hispanics/Latinos
- Adults over 60 years old
- Adults with a family history of glaucoma
- Diabetics
How is glaucoma treated?
There is no cure for glaucoma, but its damaging effects can be reduced. The disease is commonly treated by lowering or regulating eye pressure.
Doctors primarily use three different methods to accomplish this:
Medication
Prescription medication is typically the first treatment that eye doctors recommend when treating glaucoma. There are many drugs that work to lower eye pressure, but most doctors prescribe eye drops or pills. Some drugs lower the amount of fluid the eye produces, while others help fluid drain from the eye.
Some patients may experience side effects from glaucoma medication such as eye redness, stinging, or irritation. Discuss the potential for side effects with your doctor — you may need to try several different prescriptions before you find a treatment that you’re comfortable with.
Unless you have a severe allergic reaction, do not stop taking eye drops for glaucoma without consulting your doctor. Discontinuing the use of medication can increase the potential for optic nerve damage and permanent vision loss.
Laser Treatment
Selective Laser Trabeculoplasty (SLT) is often recommended for patients with open-angle glaucoma when eye drops are not effective in lowering eye pressure or if they cause uncomfortable side effects.
SLT is a painless procedure that’s performed in your doctor’s office. A special lens is used to apply an intense beam of light to the drainage system of the eye. This helps stimulate the surrounding eye tissue, so it is more effective at draining fluid and lowering eye pressure levels.
Eye pressure is often significantly reduced as a result of SLT. Many patients are able to eliminate their eye drops or use them less frequently after the procedure. The effects of SLT treatment usually last for 1-5 years and the procedure can be repeated.
Micro-Invasive Glaucoma Surgery (MIGS)
Micro-invasive procedures are proven to be extremely successful at reducing intraocular pressure (IOP) in glaucoma patients, and they involve a much lower degree of risk than traditional surgery.
MIGS procedures utilize one of three approaches:
- Increase fluid outflow using the eye’s drainage system
- Shunt fluid outside the eye
- Decrease the amount of fluid the eye produces
Trabeculectomy Surgery
Trabeculectomy surgery is a traditional approach to reducing eye pressure that has been performed for many years — usually when medical and laser treatments have failed. During surgery, a new channel is created for fluid to drain from the eye and eventually be absorbed by the surrounding tissue.
The procedure is effective in reducing IOP 60-80% of the time. There are, however, risks and complications associated with trabeculotomy surgery such as infection, bleeding inside the eye, vision loss, and low eye pressure.


The right time for cataract surgery depends on how much your cataracts are affecting your daily life—not just what they look like on an exam.
You may be ready for surgery if you’re experiencing:
• Blurry or cloudy vision
• Difficulty driving, especially at night
• Trouble reading or seeing screens
• Glare or halos around lights
• Colors that look faded
Today’s cataract surgery is safe, advanced, and customizable—with laser cataract surgery, we can restore clarity and even reduce your need for glasses.
If your vision is interfering with the things you love, it may be time to explore your options. 👁️✨ ... See MoreSee Less
0 CommentsComment on Facebook
Your annual eye exam is not only good for your eye health but can often be the first to detect other health issues as well. If it's been over a year since you have had your eye exam, February is a great time to come in and see us!
Did you know we have a new location in Kailua? ... See MoreSee Less
0 CommentsComment on Facebook
#TipTuesday
We want to ensure we are partners in your vision care. You can take steps to care for your vision, and we are here when you need us! ... See MoreSee Less
0 CommentsComment on Facebook
If you rely on eye drops all day and still feel dry, irritated, or gritty—there’s more we can do.
Dry eye is often caused by underlying issues like meibomian gland dysfunction or inflammation. That’s why we offer advanced dry eye treatments that go beyond drops to address the root cause and provide lasting relief.
Because real relief doesn't always come from a bottle. Call us today to schedule your exam. ... See MoreSee Less
0 CommentsComment on Facebook
Did you know glaucoma can often be treated at the same time as cataract surgery?
For qualifying patients, minimally invasive glaucoma procedures (MIGS) can help reduce eye pressure and medication use—while also restoring clearer vision.
One procedure. Two benefits. 👁️✨ ... See MoreSee Less
0 CommentsComment on Facebook
Retina care is one of our foundational services for our patients. Do not overlook these symptoms. Call us today if you are experiencing any of these so we can care for your vision. ... See MoreSee Less
0 CommentsComment on Facebook